The human body is a complex network of interconnected systems, each relying on the other for optimal function. Among these, the thyroid gland plays a vital role in regulating metabolism, energy production, and overall health.
However, when mitochondrial dysfunction occurs, it can have a profound impact on thyroid function, leading to various thyroid disorders.
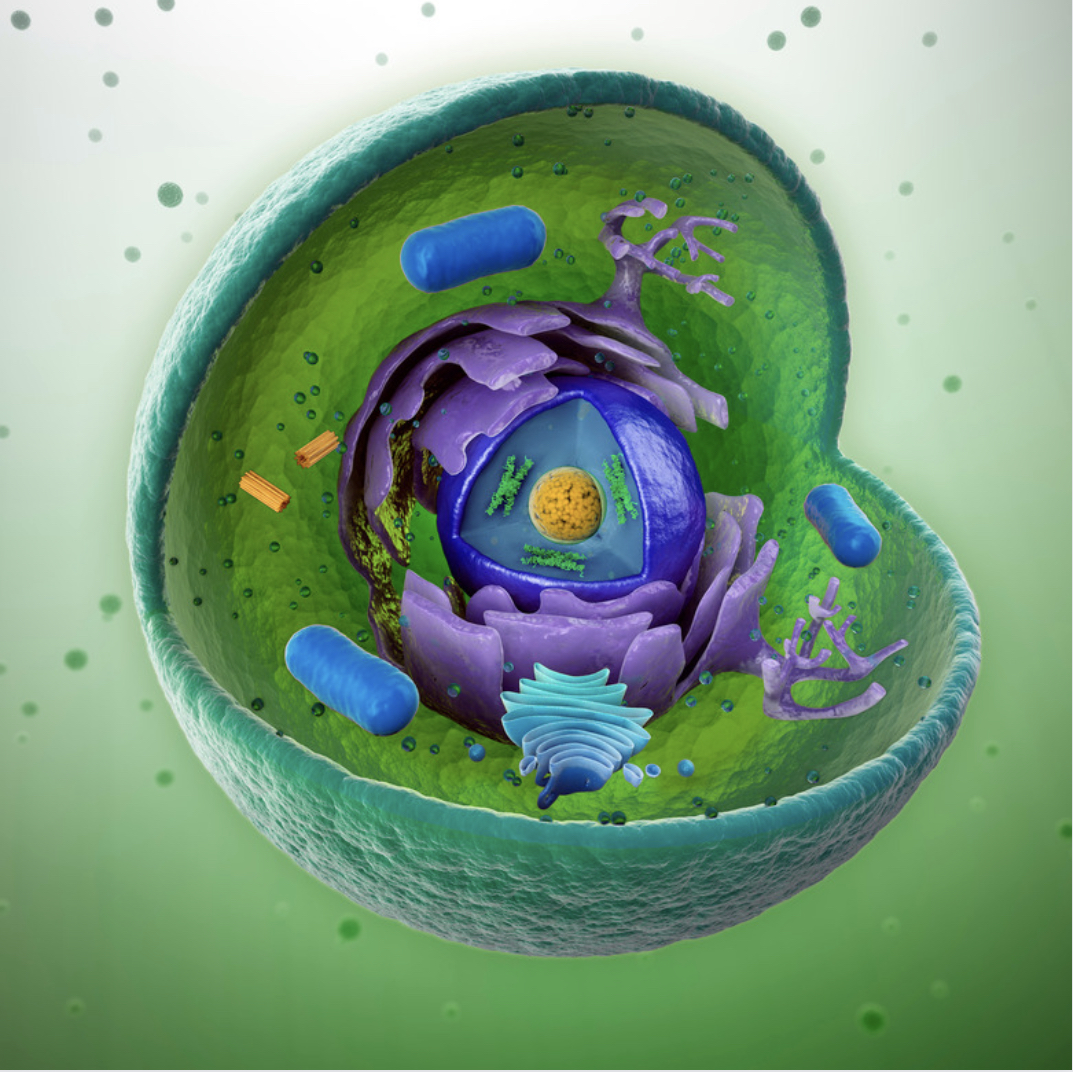
Mitochondria are often referred to as the “powerhouses of cells” because they are responsible for generating the majority of the body’s energy in the form of adenosine triphosphate (ATP).
These tiny organelles play a critical role in the production of ATP through oxidative phosphorylation, a process that relies on the transfer of electrons along the mitochondrial respiratory chain.
Mitochondrial dysfunction occurs when these organelles fail to function properly. This can happen due to genetic mutations, environmental factors, or simply as a result of aging.
When mitochondria are unable to produce ATP efficiently, it has far-reaching consequences for various bodily functions, including the thyroid gland.
The thyroid gland, located in the neck, is responsible for producing thyroid hormones, primarily thyroxine (T4) and triiodothyronine (T3). These hormones play a crucial role in regulating metabolism, body temperature, and energy expenditure. To produce these hormones, the thyroid gland relies on a steady supply of ATP, which is generated by mitochondria.
When mitochondrial dysfunction occurs, it can disrupt the thyroid gland’s ability to produce and release thyroid hormones. Several mechanisms contribute to this disruption.
Mitochondrial dysfunction results in reduced ATP production, which the thyroid gland requires for hormone synthesis and secretion.
Dysfunctional mitochondria produce higher levels of reactive oxygen species (ROS), leading to oxidative stress. Oxidative stress can damage thyroid cells and impair hormone production.
Mitochondrial dysfunction is associated with increased inflammation, which can further disrupt thyroid function.
T4 is converted into the more active T3 in various tissues, including the liver and skeletal muscles. Mitochondrial dysfunction can impair this conversion, leading to inadequate T3 levels.
One common thyroid disorder associated with mitochondrial dysfunction is hypothyroidism. In this condition, the thyroid gland fails to produce sufficient thyroid hormones, leading to symptoms such as fatigue, weight gain, and cold intolerance.
Mitochondrial dysfunction exacerbates these symptoms by reducing the energy available to the body.
Addressing thyroid disorders in individuals with mitochondrial dysfunction requires a multi-faceted approach.
Strategies to support mitochondrial health through nutrition, exercise, and supplements may be beneficial.
In cases of severe thyroid dysfunction, synthetic thyroid hormone medications may be prescribed.
Antioxidants can help mitigate oxidative stress associated with mitochondrial dysfunction.
Lifestyle changes and anti-inflammatory medications may help reduce inflammation.
In conclusion, mitochondrial dysfunction can significantly impact thyroid function, leading to thyroid disorders such as hypothyroidism.
Understanding the intricate relationship between mitochondria and the thyroid gland is crucial for effective diagnosis and treatment.
A holistic approach that addresses both mitochondrial health and thyroid function is essential for managing these conditions and improving overall well-being.